By Dylan Coombs ND and Nathan Leong M.OMSc
What is Andropause?
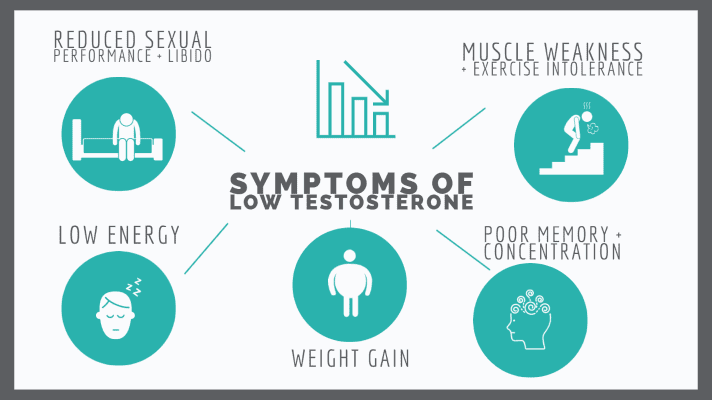
The symptoms are familiar to many men: low energy, weight gain, weakening muscles, reduced sexual performance, poor memory and concentration… Often, men chalk up these changes, and a variety of illnesses, to the inevitable result of “getting old.” It’s true that these symptoms commonly occur with age, but often they point to a specific and treatable condition. Andropause is the term for the changes that happen in men as they age, caused by decreasing testosterone levels. While it’s sometimes called “male menopause,” it is a much more gradual process which does not involve the end of fertility. Because of its slow onset, andropause is often overlooked as a potential cause of symptoms, which keeps men from finding treatments.
Testosterone drops as we age
Starting from the age of 25, testosterone levels drop about 1% every year. Although this is a natural process, it can cause testosterone levels to reach a critical low in mid-life and beyond. One in 10 men in their 50’s and one in three men in their 60’s have clinically low testosterone levels. This leads to increased fat, decreased muscle and bone mass, and reduced mental focus, energy and libido. Low testosterone is also associated with diabetes, anemia, osteoporosis, and infertility.
Bioavailability matters
Testosterone travels in the blood in forms either accessible to the body, known as “bioavailable”, or bound to a protein called Sex-Hormone Binding Globulin (SHBG). SHBG allows the body to control the amount of active testosterone circulating at any time; when the body makes too much SHBG, it binds more testosterone and effectively decreases the amount of testosterone your body has access to, even if you are still producing normal amounts. SHBG levels increase as we age, adding to the impact of andropause.
Fat and testosterone: a vicious cycle
Obesity may also cause a drop in testosterone levels. This sets up a vicious cycle, where lower levels of testosterone increase fat mass, and more fat further drops your testosterone. Additionally, fat contains an enzyme that converts testosterone into estrogen. Although men need some estrogen, it has to be in balance with testosterone. The effect of obesity in lowering testosterone while increasing estrogen pushes the body off balance from both directions.
More than just testosterone
Although the main player in men’s hormonal health is testosterone, there is a complex network of hormones and processes affecting how we feel. Dihydrotestosterone (DHT) is a derivative of testosterone that acts like its evil twin. It doesn’t provide the benefits to strength, energy or sexual function that testosterone can, but instead is responsible for male pattern baldness and prostate enlargement. If the body is shuttling too much testosterone into DHT, the hormone that you want is getting stolen and converted into a form you don’t want. Human growth hormone is another important element, helping the body create muscle, strengthen bone, and improve exercise tolerance.
Testing for “T”
So what can be done about testosterone levels as we age? The first step is getting a clear picture of what’s going on. A proper assessment of testosterone levels, including how much is actually bioavailable, will help guide whether the approach should focus more on increasing testosterone, preventing its conversion to undesired molecules, or limiting how much of it is locked up and unavailable for use. Each of the measures of testosterone has an ideal range that depends on other factors to interpret; picking treatments without the full story is inefficient at best and dangerous at worst. Further investigation would measure organic acids to see the products of each step of the hormone pathway, determining where the process is breaking down. Once it’s clear why your body isn’t able to access all the testosterone it needs, treatment options become more clear. Because low testosterone can mimic so many conditions, it’s also critical to rule out other causes of fatigue, sexual and memory problems at this stage, to make sure focus is put on the most beneficial treatments.
Treatment approaches
No matter the cause of andropause, exercise will always be part of the cure. If excess fat is a contributing factor, decreasing fat can improve testosterone levels and reduce estrogen to re-balance the hormone ratio. Beyond weight changes, all forms of exercise can benefit mood and energy, balance blood sugar, and decrease the risk of heart disease. Resistance exercise is especially beneficial, as it builds muscle and strengthens bone, while there is evidence that squats in particular can directly increase testosterone levels. If the main cause of andropause is high SHBG levels, herbal and supplement options are available to free up more of the testosterone the body is already making. Food choices are also important, as diets very low in calories or protein can each cause high SHBG. When a particular step in the formation process is failing, vitamins and supplements can support the output of that particular enzyme. For those who can’t digest the vitamins and minerals they need, IV solutions will help to increase levels. If the body doesn’t respond to supportive treatments, or is failing to produce any testosterone on its own, a referral to a practitioner who can prescribe pharmaceutical testosterone may be necessary.
Osteopathic perspective: body motion dictates function
In osteopathy, we look for structural problems that are impairing homeostasis, and correct them through gentle movements and exercise advice. We all have a continuous layer of fascia (skin) covering our body, including the hips and legs. This layer has many connective tissue attachments to the internal organs, including our reproductive organs.
When we move our body regularly, the connective tissue creates heat and is mobile around the body. This keeps homeostasis and helps the body to maintain function. When we move less, the active connective tissue will begin to deposit fatty tissue and to lose mobility. When this happens, homeostasis is lost, and the body instead turns to sympathetic “fight or flight” responses, which can affect hormone health. Osteopathic treatments to restore function in connective tissue can improve reproductive balance.
Next steps
Andropause is a complex diagnosis but can be managed effectively. If you have been told you have low testosterone, or these symptoms match your experience, I encourage you to reach out for further assessment. With a condition that is impacted by – and can have effects on – so many parts of your life, a full investigation and multi-factor approach is needed to get you back to feeling your best.